UMC Utrecht generously rewarded by KWF
In what ways can immunotherapy be used more effectively against head and neck cancer, liver cancer, multiple myeloma and other tumor types? And how do we prevent children with thyroid cancer from being overtreated? These questions are being investigated in four new studies at UMC Utrecht. KWF Dutch Cancer Society is funding these projects, about which we tell you more below, with over three million euros in total.
1.Fortified army of immune cells
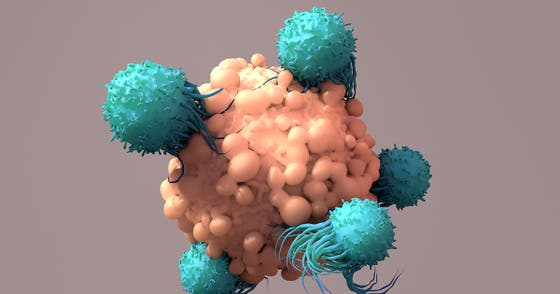
Our body is one huge battlefield: it’s constantly fighting all kinds of invaders, often without us even realizing it. Just think of viruses, bacteria, fungi but also cancer cells… Our army of T-cells (a special kind of white blood cells) waits for them and clears them away. Our ingenious self-defense mechanism serves as the basis for designing immunotherapy. This treatment activates and strengthens our immune system. Physicians are already successfully using immunotherapy against a variety of illnesses.
There are several ways to produce immunotherapy. Researchers can, for instance, multiply the body's own T cells. But researchers can also slightly genetically modify the body's own immune cells, allowing them to fight the battle in a more targeted way. The latter is the case with, for example, TEG therapy, which is the focus of one of the new studies.
TEGs are genetically engineered T cells that combine the best of two types of T cells (alpha-beta and gamma-delta cells). Patients’ own immune cells are taken from them, modified and then returned to them. The enhanced army of T cells can then recognize and eliminate cancer cells more quickly and effectively. TEGs were invented and developed at UMC Utrecht by Jürgen Kuball (professor of hematology at UMC Utrecht) and his research group.

Jürgen Kuball
First and second generation
In their previous experiments at the cellular level and in mice, the researchers have shown that treatment with this form of immunotherapy is safe and effective. And TEGS are now also being tested with humans: this year, the first complete remission was observed in a leukemia patient during a clinical trial. This certainly gives great hope for further application in humans.
On the basis of these initial results, Jürgen will now start developing the second generation of TEGs. KWF has granted him 775,000 euros to help him do so. He is going to enhance the TEGs with different and more proteins now. This will make them even more effective. The new generation will be able to recognize more types of cancer. That is, some tumors are being protected by their own powerful 'firewall'. This is especially the case with solid tumors (cancer in organs and tissues).
Jürgen and his team also would like the second generation to remain active longer and in greater quantity, to control the tumor better and to stimulate other immune cells. In mice, the first positive results have already been achieved: tumors started to shrink, while healthy cells were not at risk.
Jürgen is now focused on devising a treatment for patients with head and neck tumors. This type of cancer is rare, often diagnosed at a late stage and therefore difficult to treat. He hopes that this more powerful TEG will help to initiate clinical trials for patients with head and neck cancer more quickly. In addition, he expects that this improved therapy could also work with other types of cancer.
"We are now developing T cells that are more resistant to the defense mechanisms of cancer cells. This is currently a major challenge in treating cancer with immunotherapy," Jürgen says. "Research on the first generation of TEGs is certainly continuing, because we have found them to be effective. The next generation of TEGS is a good addition, but of course we will first thoroughly investigate whether our ideas really work and that they are safe before testing them in patients."
2. Boosted CAR-T
With his new research, associate professor Victor Peperzak is trying to improve CAR T cell therapy for multiple myeloma patients. To that end, KWF and funding partner Alpe d'HuZes have granted him over 850,000 euros.
Like TEGs, CAR T-cell therapy is a form of immunotherapy in which T cells are genetically modified. With this specific treatment, T cells are taken from patients, genetically altered into CAR T cells and returned to them. The genetically modified immune cells carry a special protein that acts like a sort of ‘antenna’: as soon as it recognizes the cancer cell, it immediately sounds the alarm. As a result, CAR T cells can clear tumors sooner and better (and provide protection longer) than non-adapted T cells.
AR T-cell therapy is already being used successfully with a number of blood cancers. But the disease, unfortunately, often returns after treatment. This is especially true for people with multiple myeloma, a rare form of bone marrow cancer in which plasma cells proliferate. Plasma cells are a special type of white blood cells that produce antibodies.

Victor Peperzak
Toxic molecule decides battle
Victor and his research group now would like to improve the way CAR T cells kill cancer cells. They have already shown in a previous study that genetically modified immune cells can be additionally armed with NOXA. This is a toxic molecule that is specifically released into myeloma cells and kills tumor cells there.
In the new research project, Victor and his team would like to determine how to produce and apply the enhanced CAR T-cell therapy as efficiently as possible. Furthermore, they want to see if the new therapy works better in multiple myeloma than the existing CAR T-cell treatment. Finally, they would also like to make sure healthy tissue will not be damaged by adding NOXA. To this end, they will test the new treatment at the cellular level, in mice and in 3D culture models with bone marrow cells from myeloma patients.
This study is intended to serve as the basis for a new clinical trial to be set up in myeloma patients.
"CAR T-cell therapy initially gave tremendously encouraging clinical results with myeloma cells. In almost all patients, the cancer cells were cleared and seemed to be gone, but, unfortunately, they returned after some time," Victor says. "Therefore, we developed this method to allow CAR T cells to also diminish the more resistant myeloma cells. We expect that this enhanced CAR T-cell therapy will work more efficiently and will prevent or delay cancer recurrence."
3. Proteins on the move
Assistant professor Dennis Beringer, who is part of Jürgen Kuball's research group, focuses on so-called GABs. These are therapeutic proteins that connect T cells with tumor cells, allowing the cancer to be detected and addressed more quickly. Dennis will receive over 790,000 euros from KWF.
GABs can be produced faster, easier and cheaper than the earlier mentioned TEGs. The latter indeed show promising results, but they are still more difficult and expensive to make. That is, TEGs must be developed per individual patient, which is time-consuming and makes large-scale production difficult.
GABs, on the other hand, can be produced more easily and less expensive in greater numbers. As a result, more patients could be treated more quickly at a lower cost. During previous research focused on leukemia, Dennis and his colleagues have already developed GABs with promising results: cancer cells were recognized faster, and tumor growth in mice was slowed down.

Dennis Beringer
Liver tumor organoids
Now, Dennis is going to improve these GABs, helping T cells to signal and eliminate a wider range of cancer cells. In doing so, he is working primarily with liver tumor organoids. Organoids are mini-organs or tumors that have been grown in a laboratory. The organoids in this study were made available by the research group of principal investigator Weng Chuan Peng at the Princess Máxima Center for Pediatric Oncology. Dennis' goal, however, is to use the improved GABs to develop immunotherapy for various types of cancer, both solid and non-solid types, not just against liver cancer.
Dennis will now first determine how to get the GABs to bind to tumor cells as well as possible, so that fewer are needed for the same effect. Then, he is going to add another protein to the GABs, making the T cells even more active.
"For many cancers, immunotherapy does not yet work optimally. So, developing new strategies and improvements is very important to eventually be able to treat a larger group of patients with immunotherapy," Dennis says. "We hope that the improved GABs will eventually be tested in patients. There are still some important steps needed to prove that the GABs are effective and safe. After that, preparations for a clinical trial can begin."
4. Stop overtreatment of thyroid cancer
Thyroid cancer in children is very rare, affecting 10 to 15 children annually in the Netherlands. Fortunately, with current treatments, children with this type of cancer have a good survival rate of more than 98 percent.
Standard treatment includes removal of the thyroid gland and subsequent administration of radioactive iodine. Unfortunately, over 40 percent of children subsequently experience adverse effects from the given treatment, such as parathyroid, salivary gland and tear duct damage. They may also have an increased risk of developing second tumors. Furthermore, they’re often tired and have problems concentrating.
The good prognosis of 98 percent combined with the many side effects suggests that many children are now being overtreated. With some children, a less intense treatment may be sufficient, leaving them with fewer side effects. But who can be treated less intensely, and which children should receive the heaviest treatment? Sarah Clement (pediatrician and postdoctoral researcher in pediatric endocrinology) hopes to answer this question with her research project for UMC Utrecht’s Thyroid Cancer Center of Expertise. For this, KWF has awarded her the Young Investigator Grant of over 760,000 euros.

Sarah Clement
International cooperation
The solution for children’s overtreatment can be found in developing reliable predictive models, Sarah believes. With these models, the risk of return of the disease can already be determined during diagnosis. Drawing up these models requires a lot of data from patients. This is difficult because it’s such a rare disease, with only a small number of annual new patients in the Netherlands.
That's why Sarah, together with Hanneke van Santen (associate professor of pediatric endocrinology at both UMC Utrecht and Princess Máxima Centre), set up a unique European registry for children with thyroid cancer last year: the ped-DTC registry. With KWF's grant, the first predictive study (ped-DTC STRATIFY) within this registry will now be conducted.
Over a two-year period, 200 European children with recently diagnosed thyroid cancer will be added to the study. The researchers will record the characteristics of the thyroid cancer and the treatments given. And they will also be tracking notable genetic changes in the removed thyroid tissue.
The patients will be followed for 24 months after their diagnosis. By closely comparing the collected data and the eventual recurrences of the disease, Sarah and her colleagues aim to signal the specific factors determining the return of thyroid cancer. This way, it will be possible to clarify, for each child, whether the risk of recurrence will be high before starting treatment. This will help their doctors to decide which children they’ll need to give more aggressive treatment and which patients will be better off with less intense therapy. In the latter case, surgery may be less extensive, or the use of radioactive iodine may be omitted.
"Due to the lack of prospective studies, all children with thyroid cancer have been treated almost the same for decades," Sarah says. "Thanks to the KWF grant and our unique European collaboration, we are now able for the first time to develop an adequate model to estimate the risk of recurrence at diagnosis. The ultimate goal is to use this model to personalize the current treatment strategy so that children with and beyond thyroid cancer will have a better quality of life."
